Madison was ill with various upper respiratory
infections throughout much of last winter and into the spring of 1999.
She had been treated in early May for supposed "pneumonia"
with two rounds of antibiotics. Then on Tues., July 13, 1999, Madison
awoke with fever, very shallow breathing and complained that her
"side hurted". After a trip to the ER, a chest x-ray and
radiologist revealed "probable pneumonia". Again we tried
antibiotics--2 courses—to no avail. Soon, Kathy and Steve realized
that Madison was indeed, getting worse instead of better. During the
week of July 19, 1999 Madison’s previous symptoms increased
ten-fold. In addition to the fever, shallow breathing and abdominal
pain, she also became very withdrawn, lethargic, dehydrated, had a
distended tummy, and had very decreased appetite. Previously we had
been told by our former pediatrician that her symptoms were not
uncommon with pneumonia. The other symptoms we identified were
down played by our pediatrician. However, under pure frustration we
brought Madison into the "Pediatric After Hours Clinic" on
Sunday July 25, 1999 for another opinion. Immediately they identified
her very enlarged liver in addition to "pleural effusion"
(liquid trapped on the outside of the lung – compressing against it
and only allowing her rapid / short breaths). Madison was admitted
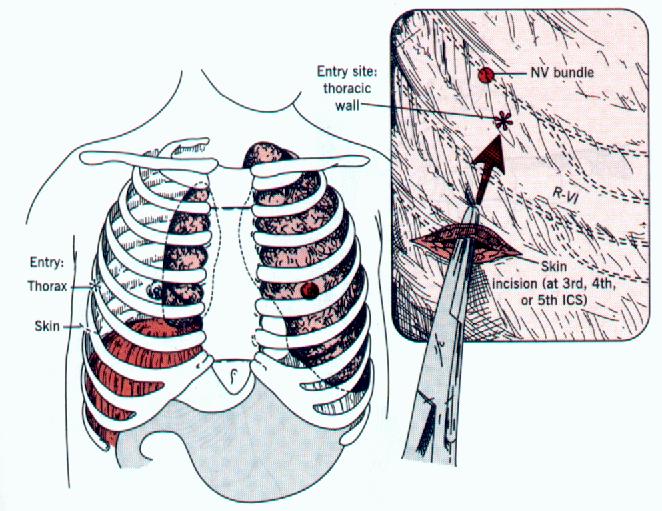
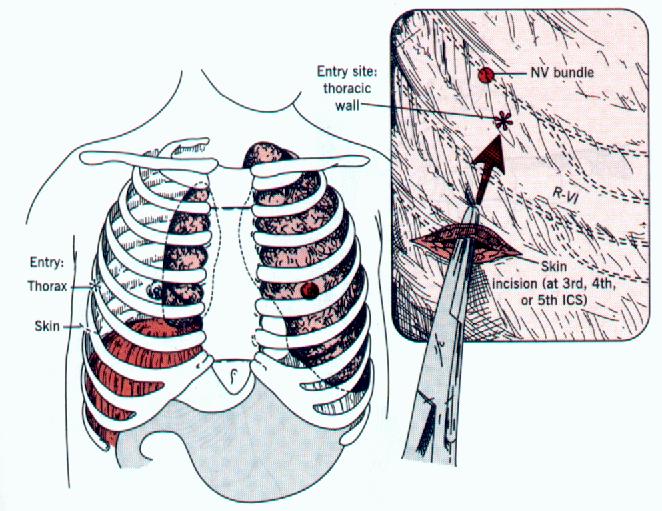
into the hospital immediately. On Mon., July 26, a pleurocentesis
procedure was performed (insertion of a hollow needle into the pleural
cavity--space between the chest and lungs-- through the chest wall in
order to withdraw fluid, blood, pus or air). A significant amount of
yellowish fluid was withdrawn from her chest giving her temporary
relief so she could breath at a much more normal rate. She was also
catheterized and began an IV. Perhaps the most important piece of
information obtained on 7-26-99 were the results of Madison’s
bloodwork—which showed her to be anemic with a hemoglobin of 7.6
g/Dl. This prompted additional bloodwork to find the cause of anemia
and low hemoglobin count.
Madison was transferred to the Pediatric Intensive
Care Unit (PICU) so she could be more closely monitored. Madison was
then hooked up to monitors tracking her oxygen level, heart and
breathing rate. She also had portable chest X-rays performed to
identify or better diagnose her condition. Blood was withdrawn and
labs sent out to understand the chemistry behind her weakened status.
However, throughout the day Madison’s breathing rate and oxygen
levels started to diminish. She then needed an oxygen mask to help
supplement her intake and ensure her body received enough to keep her
alive. During the late hours of July 26 and early hours of July 27
Madison’s breathing rate was putting her into a more critical
category. It was decided that the rate of fluid generation (‘pleural
effusion’) was out-matching her ability to remove fluid normally and
that the insertion of a chest tube would be necessary. The tube would
then allow drainage of the fluid in the outer chest cavity and remove
the pressure from her lungs, thus allowing her to breathe better. This
was performed in the early hours of Tuesday, July 27. See the figure
below.
After the chest tube Madison improved slightly,
however, she was still required to be on oxygen and under constant
care. Around 10 am on July 27, 1999 Madison was taken to have a CT
scan of her chest and abdomen area. Madison was sedated for this
procedure. Ironically, on the way down to the CT room the first hint
of CANCER was mentioned – but in the pediatrician’s own words
"it would be almost unlikely" – just a precautionary
statement.
The
afternoon of July 27, 1999 was when the world came crashing down on
us. Approximately fifteen doctors including nursing staff and a
psychologist came into Madison’s room to update us on the CT scans.
Leading the discussion was the hospital’s primary oncologist, Dr.
Kulkarni, who, in a very straightforward and compassionate manner,
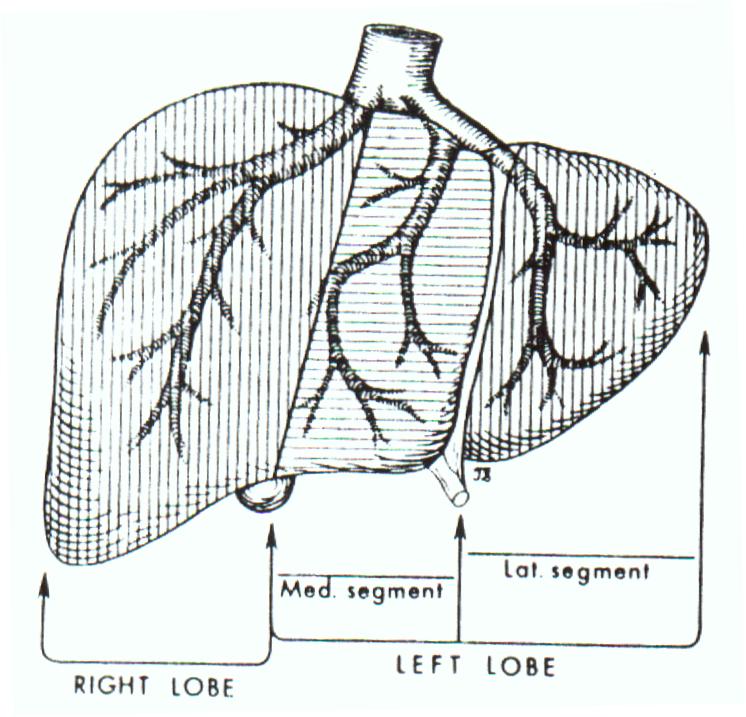
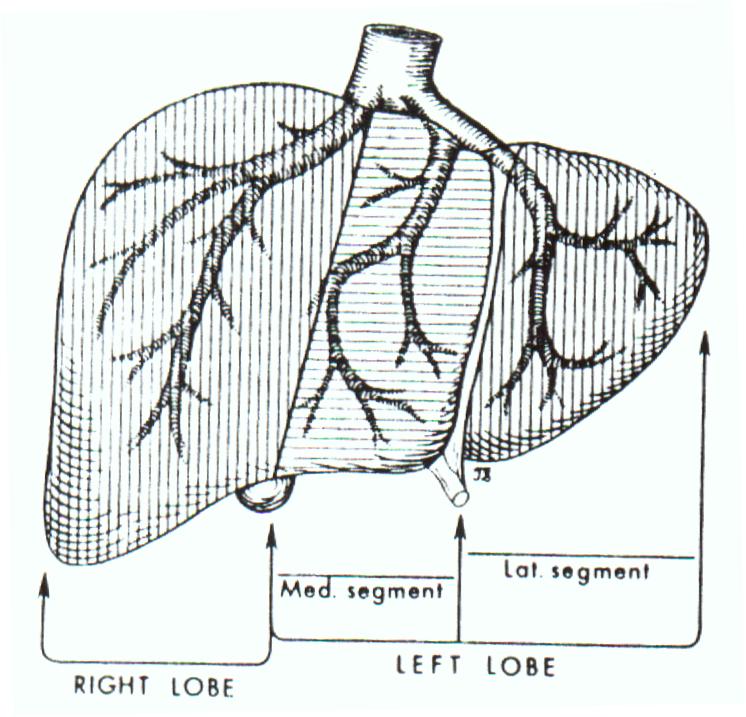
informed us that Madison had Hepatoblastoma – Stage IV. The CT Scans
identified a very large tumor in the liver (see figure below) , a mass
in the right atrium of the heart, approximately 6 to 12 tumors on each
of the lungs and a tumor impacting the IVC. Additionally, an alpha
fetoprotein (AFP) level came back very high. AFP is a protein that is
elevated in the blood of children with liver cancer. In healthy
children the AFP is below 10 ng/ml; however, in Madison’s case it
was 832,240 ng/ml.
Madison was in Kathy’s arms and still lethargic
from sedation. Obviously she couldn’t comprehend the verdict handed
out to her. As her parents, nothing could’ve prepared us for this
nightmare—we were numb, grief-stricken and terrified. We both prayed
for the doctors to return to our room and say they made a mistake and
misread the scans. We were in a haze – a fog.
That afternoon Madison was scheduled for emergency
surgery to install her Broviac line. This line was inserted into the
superior vena cava, which draws off the area around the heart and
comes back out the chest. You will see this in her videos that are
attached in the education section. This line replaces the IV and
allows blood to be drawn from Madison without a needle. It also allows
for the injection of chemo drugs and if necessary the site where Total
Parental Nutrition (TPN – liquid nutrition / food) can be
administered. That night Madison was given a cardiogram (an ultra
sound of the heart) to obtain a baseline size of the right atrium
tumor. Its longest dimension was 3.28 cm and thankfully was not
impacting the valve function.
Madison spent a total of 21 days